Drug-resistant bacteria or Anti-Microbial Resistant (AMR) bacteria can become a global health issue. A review conducted in 2016 projected that by 2050, as many as 10 million people could succumb to AMR bacteria per year across the world. If the situation continues without any intervention, diseases that were curable with a few days’ use of antibiotics would be challenging to cure further, thus increasing global mortality due to AMR.
In a similar study published in Lancet recently, the threat of AMR bacteria has once again been highlighted. The Lancet study, one of the most comprehensive global analyses on AMR bacteria, found that in 2019 alone, 4.95 million people died from diseases where AMR bacteria played a role. Out of these, 1.27 million deaths were ascribable to direct results of AMR. This indicates that AMR caused more deaths than HIV/AIDS or even malaria in 2019. The global deaths related to HIV/AIDS and Malaria were 864,000 and 643,000, respectively.
The lancet research involved several scientists. Mohsen Naghavi, one of the authors of the study and a health metrics scientist at the University of Washington, commenting on the findings said, “AMR is truly a global problem that requires urgent action from policymakers and the health community to avoid preventable deaths.” He further added, “In a world where antibiotic use has become so commonplace, resistant bacteria out-compete those that are killed off by pharmaceuticals.” The bacteria that are resistant to antibiotics is on a steep rise, posing a global concern for health experts worldwide.
Naghvi and his teammates used data from the 2019 GBD (Global Burden of Diseases, Injuries and Risk Factor) study, also published in Lancet in October 2020. The GBD study surveyed 369 diseases and injuries in 204 countries and territories. The study considered people of all ages to assess the number of people who died from infections globally, and the pathogens (agents that cause diseases) responsible for the diseases coupled with other factors. Naghvi and his team used all the available data on AMR to find the prevalence of AMR in several locations and the correlation between AMR and mortality.
In their analysis, the research team found that in 2019, as many as 1.27 million deaths globally were directly caused by AMR bacteria. Moreover, the study also revealed that this number was associated with AMR more than twice.
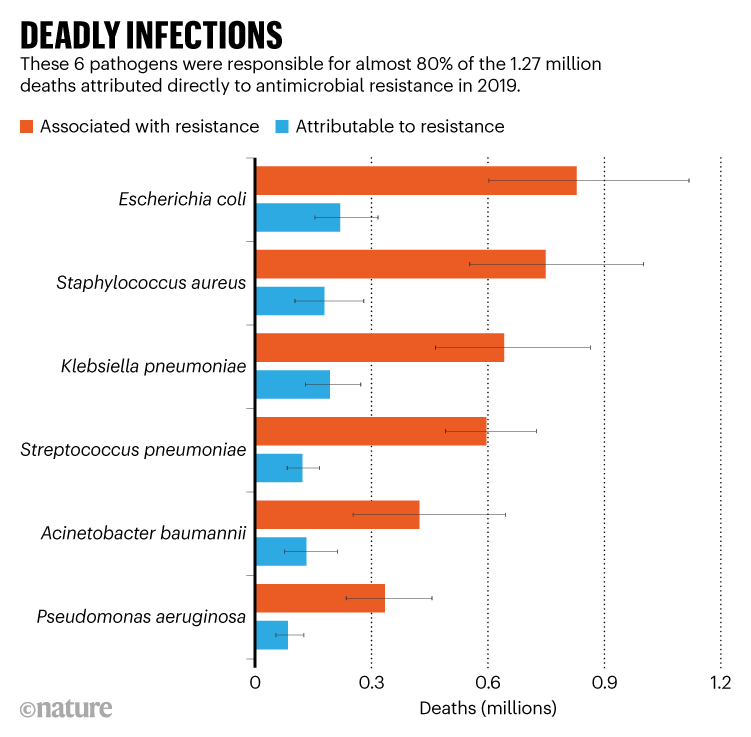
It was further found that the most common sites of infection caused by AMR bacteria are the chest, abdomen and bloodstream. Infections in these parts were found to be in 78.8% of deaths directly related to AMR. Six such deadly bacterial pathogens were responsible for three-quarters of all the deaths linked to AMR. The E. Coli that is resistant to antibiotics was found to have caused the deaths of about 200,000 people in 2019 as well.
Image depicts AMR bacterial pathogens and the deaths caused by them. Image source: Nature, used for representative use only.
The Lancet research also found that lower-income countries were the worst sufferers of deaths from AMR bacterial pathogens. Among the regions considered for the study, Sub-Saharan Africa registered the highest death rate directly attributable to AMR. 27.3% of 100,000 people died in this region due to AMR. Worryingly, the prevalence of AMR bacteria and the number of infections were higher in low-income countries than the wealthier ones. Commenting on the regional variation of AMR deaths, Naghvi said, “Regional estimates are useful for policy planning specific to the challenges faced by each region. One-size-fits-all approaches are unlikely to be appropriate.”