The recently released findings of a UK public inquiry confirmed that during the 1970s and 1980s, 33,000 British citizens were infected with HIV or Hepatitis C through blood transfusions, resulting in around 5,000 deaths. The inquiry found that contaminated blood products were imported from the United States and bought from commercial blood banks that did not test the “merchandise” for possible contamination.
The report caused a political scandal, prompting Prime Minister Rishi Sunak’s government to promise compensation to thousands affected. However, victims’ families are not satisfied and plan to sue the state for more reparations, potentially amounting to billions of pounds, according to the BBC.
Brazil recorded similar cases when blood products were commercially traded. The famous story of brothers Betinho, Henfil, and Chico Mário, who contracted HIV this way, led to significant reforms. Betinho, the only brother to survive into the 1980s, founded the Brazilian Interdisciplinary AIDS Association (ABIA), partly to advocate for safer blood transfusion practices. This struggle resulted in the Henfil Law, mandating laboratory blood testing, and the Betinho Law, banning the sale of blood, according to Veriano Terto Júnior, vice-president of ABIA.
Today, economic interests aim to resume the purchase and sale of blood derivatives through a proposal to amend the Constitution – known as the Plasma PEC – which has received Senate Committee approval. Its advocates argue it would prevent alleged “blood wastage”. However, since the introduction of the Henfil and Betinho Laws, Brazil has developed alternatives: the Brazilian Hemoderivatives and Biotechnology Company (Hemobrás), a public company founded in 2004.
Recently, Hemobrás inaugurated a plant in Goiana, Pernambuco, to manufacture Factor VIII, the protein imported carelessly and responsible for many infections in the UK. Importantly, Factor VIII will be produced as a biotechnological, not a blood product. Ana Paula Menezes, innovation director at Hemobrás, discussed the company’s production capacities and expansion plans announced by the current management in a conversation with Outra Saúde. According to Veriano, strengthening Hemobrás is a better path than “returning to the barbarity of the times when blood was a commodity.”
How it was in Brazil
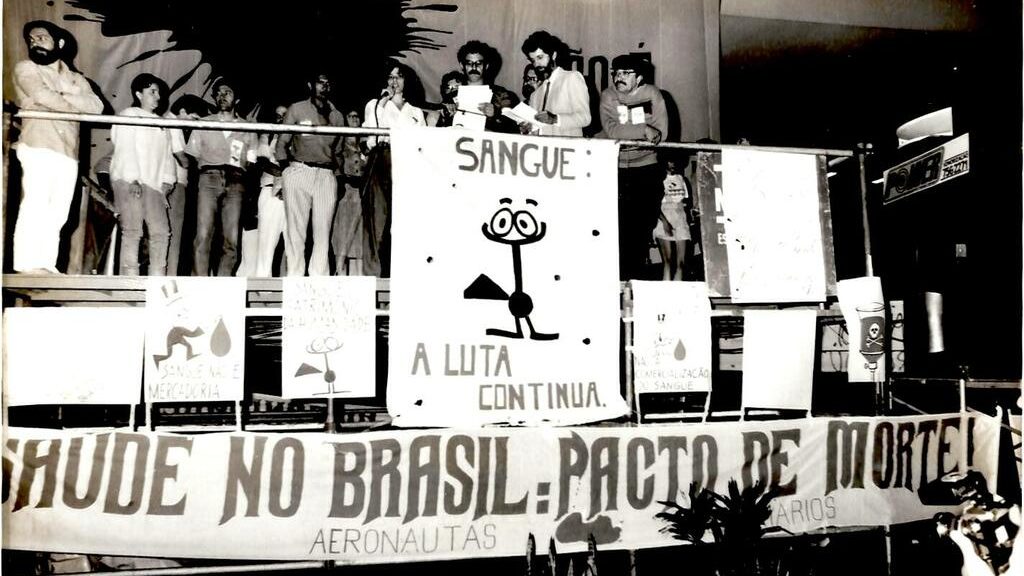
ABIA’s recent newsletter, “The Return of the Vampires,” recounts the history of the “Blood Pact” campaign, which influenced the 1988 Constitution. Under the slogan “Blood is not a commodity” and with illustrations by the cartoonist Ziraldo, the campaign ensured the inclusion of paragraph 4 in article 199, prohibiting “any kind of commercialization” of the “collection, processing and transfusion of blood and its derivatives,” according to Richard Parker, director of ABIA.
Veriano Terto recalls that prior to this, blood transfusions and access to blood products were handled negligently, “without regard for human life.” Additionally, misinformation linked AIDS transmission to homosexuality rather than improper handling of blood and transfusions.
The unity between the health reform movement and the AIDS movement was crucial in this scenario. The 1986 National Health Conference discussed the issue of blood, and these movements linked national sovereignty (protection of Brazilians’ blood) with the reality of the AIDS epidemic, which was affecting thousands, many marginalized from society. Parker’s article highlights how these organizations “articulated the notion of solidarity as a kind of ‘vaccine’ against the symbolic violence of AIDS-related stigma and discrimination.”
In the same year that the Constitution was announced, the Henfil Law was passed, requiring the testing of collected blood—precisely what had not been done in the UK, leading to the infection of 33,000 people. The impact of this law in the fight against AIDS was significant.
“The enactment of the Henfil Law allowed Brazil to reduce HIV transmissions through blood transfusions to negligible levels, less than 1%,” Veriano says. A few years later, the Betinho Law was passed, regulating the constitutional provision and permanently ending the commercialization of blood.
The post-Hemobrás scenario
Despite advancements represented by mandatory testing of collected blood, Brazil was not self-sufficient in blood and blood products during the 1990s and relied on international trade to maintain its supplies.
“Brazil was completely dependent on foreign purchases. We lacked access to production processes and were at the mercy of market prices, with no benchmarks for regulating prices for SUS purchases,” says Ana Paula Menezes.
To address this, Hemobrás was founded in 2004 during Lula’s first administration. “The aim was to ensure Brazil could produce blood-derived and biotechnological medicines domestically for SUS users, guaranteeing quality and effective testing, thereby reducing dependence on foreign products,” Menezes says.
Today, the state-owned company is a “significant supplier of blood products to SUS, providing albumin, immunoglobulin, plasma coagulation factors VIII and IX, and recombinant Factor VIII, produced through biotechnology and not dependent on human plasma.”
Factor VIII deficiency causes classic hemophilia, a condition that affected Betinho, Henfil, and thousands of Britons who contracted HIV or Hepatitis C from untested blood. In April, Brazil opened a factory in Pernambuco to produce this product, enhancing sanitary sovereignty. “At the plant’s inauguration, President Lula highlighted Hemobrás’s importance for hemophilia patients, recalling Henfil and Betinho, and noting that today they might not have faced the same hardships as hemophilia patients experienced in the 1970s and 80s,” says Menezes.
The company’s deliveries are already substantial and are expected to grow with the opening of a new factory next year, capable of storing 500,000 liters of plasma. “Our current model supplies about 200,000 liters annually, a figure expected to rise with the Federal Government’s R 100 million [approximately 19 million USD] investment through PAC Saúde for equipment at blood centers to supply more industrial-quality plasma to Hemobrás,” Menezes adds.
By the end of 2026, Hemobrás aims to achieve 100% national production of blood products and recombinants, “an important step for Brazil to achieve self-sufficiency in these medicines.” This goal has earned it the Strategic Defense Company (EED) seal, recognizing its strategic value for Brazil’s independence from the foreign market. Menezes notes that not only hemophilia patients but also “ICU patients, severe burn victims, and those with kidney and autoimmune diseases will benefit.”
New challenges
Despite significant progress in recent decades, there are still shortcomings in Brazil’s public health capacity. After all, although it is in the plans, self-sufficiency has not yet been achieved. Veriano believes this gap has allowed the health business community to reintroduce the proposal to commercialize Brazilians’ blood.
This effort is embodied in the proposed amendment to the Constitution 10/2022, known as the Plasma PEC, which was approved by the Constitution and Justice Committee of the Senate last October, marking the first step toward a vote by the Congress.
The PEC aims to distort Article 199 of the Constitution, which was established through the mobilization led by Betinho and his allies. It proposes that “private blood banks be allowed to sell plasma” to “pharmaceutical companies, which would then process it and sell the resulting drugs to the private market,” according to the official interpretation.
Organizations that have supported the state-run blood management model, emphasizing public health, human dignity, and national sovereignty, are critical of this proposed change and foresee significant dangers.
Veriano raises ethical concerns about treating blood as a commodity. “Once again, private pharmaceutical companies are pressuring us to relax the law, to go back to the commercialization of blood. I’m concerned because blood is not a commodity, it is a human organ,” Veriano says. “What guarantee do we have that after commodifying blood, we won’t see the same pressures to market other organs that can be transplanted, like kidneys?”
A return to the old model, where companies are trusted to oversee and test the blood collected and sold, could cost lives. “One of the only effective measures we had to stop HIV transmission via transfusion was the Henfil Law. In a country where AIDS cases have risen again in recent years, especially among vulnerable populations, this [pressure to commercialize blood] is a threat of regression,” Veriano continues.
He concludes that Brazil’s success in controlling blood safety came only after it became the domain of SUS and the state’s responsibility, ending commercialization. “We are against any prospect of commercialization of blood or blood products until we are proven otherwise,” concludes Abia’s vice-president.
The article was written by Guilherme Arruda and published in Portuguese on Outra Saúde.
People’s Health Dispatch is a fortnightly bulletin published by the People’s Health Movement and Peoples Dispatch. For more articles and to subscribe to People’s Health Dispatch, click here.