The models chosen for financing health systems have a profound impact on how they function and to whom healthcare is accessible. Public investment in health has been long recognized as a financing model that improves access and diminishes inequalities, but it has yet to become the predominant financing model. Even in those countries that rely on public spending for health, the money often gets diverted to private providers, which undermines the potential of the model.
Even though there is a sort of global consensus that public spending is essential – not necessarily sufficient – to improve the health of people, there remain staggering inequalities in public investment across countries. Countries with higher incomes are more likely to invest in health than those with lower income. For instance, High Income Country (HICs) governments spend around $2,235 (median) per person per year on health. In contrast, average per capita government spending in Low Income Countries (LICs) is less than one hundredth of the HIC average – $22.
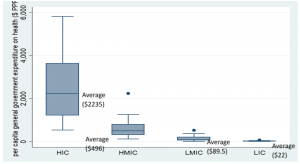
Box plot: Per capita public spending on health by country groups: 2018
Source: Author’s estimates based on WHO Global Health Expenditure database, HIC: High Income Countries; HMIC: High Middle Income Countries, LMIC: Low Middle Income Countries; LIC: Low Income Countries
More than a third of total global public investment on health is made by the US Government alone (figure 2). Yet a significant proportion of the US population does not have adequate financial protection against health events. At the same time, 56% of the world’s population lives in LICs and low-and-middle income (LMIC) countries. But their share of total public investment is only 2%. All the big economies, such as the UK, Japan, Germany, France spend many times more than their share of the global population.
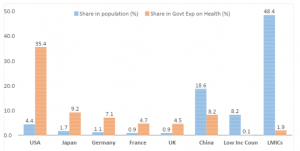
Inequalities in Global Public Spending on Health
Source: Author’s estimates based on WHO Global Health Expenditure database
Public investment on health has been regarded as the most progressive source of financing for healthcare. Progressive financing means people pay for healthcare based on their means, but access care based on their needs. Developing countries like Thailand, Malaysia, Cuba and Sri Lanka, which have been able to ensure universal access to healthcare, have used publicly financed healthcare to reduce the financial burden of households and bring down inequities in access. When public investment is low, millions of people are deprived of adequate and appropriate access to healthcare, are forced to forgo care, die untimely deaths, get pushed to poverty, face financial hardship, often sell off assets or borrow money and remain in perpetual debt. Public investment helps break the vicious cycle of poverty and ill health.
The aim is care, not coverage
The current discourse on Universal Health Coverage centers around increasing public spending on health. On the face of it, this seems to be a progressive proposition. However, the underlying assumption is that, if finances were secured, the existing mix of private and public providers could continue to be in charge of provisioning of health services. The use of the term ‘coverage’ itself, rather than ‘care’ symbolizes the move away from concerns of ownership of means of production and design of health systems towards financing. Securing public investment is seen as a way to propagate market penetration in health, rather than a means to replace it through non-commercialized provisioning.
Funding agencies are promoting a model of a general government revenue-financed system, where private insurance intermediaries are being used to purchase care from mainly private providers. Such a model was first introduced in the United States in 1965 in the form of Medicaid. Medicaid was introduced mainly as a response to the popular uprising during the 1960s. The program played a key role in providing financial protection to the poor people, in an otherwise over-medicalized, private insurance and private provider-dominated US health system.
The application of such a model in various developing countries, however, is highly problematic for various reasons. Experiences of countries such as Costa Rica, Chile, Mexico and in recent times China and India, show that such schemes not only fail to ensure financial protection for the beneficiaries, but can also cause an increase of costs.
In the US health system, a huge amount of money goes into regulation and administration – approximately a third of the total spending. About $496 billion is paid for billing and insurance related costs (BIR) in the US, more than the total public spending of 154 countries.
Public money flowing to private contractors
The existing regulations in the US fail to regulate over-medicalization and administration of unnecessary care induced by the providers, while at the same time leaving an enormous part of the population without any health care at all. Most of the public investment and private expenditure become profit for pharmaceutical and insurance giants, and Health Maintenance Organizations (HMO), networks that provide health insurance coverage. These three groups of entities control a huge part of the healthcare market and extract high levels of profit out of it. They enjoy such a level of power that they are able to exert influence on the government, policy and the media to protect their interests and profits, many times at the expense of securing adequate access to healthcare.
While the world is trying to overcome the impact of the COVID-19 pandemic, there is an urgent need to build strong health systems across the world. However, the magnitude of public investments required to meet access gaps in LIC and LMICs cannot be financed only through investments by country governments. While the developed world is putting in greater resources to health, and poorer countries are failing to sustain their existing finances, global inequalities are likely to exacerbate.
The US health system and those of many rich countries need serious reforms to curb unnecessary care, minimize profits, and give up models of over-medicalized commercialized healthcare systems. If half of the US public spending was channeled to other countries through multilateral institutions, public spending on health could be doubled in 176 countries of the world, benefiting two thirds of the world’s population.
It needs great political will to rationalize profits, if not eliminate those entirely; give up on monopolies and consider health as a global public good. By changing their model of financing, the US and other rich countries could not only improve health outcomes of their population but also save millions of lives around the world, and contribute to ensuring that the post-COVID world is really more equitable than the one we inhabit now.
Read more articles from the latest edition of the People’s Health Dispatch and subscribe to the newsletter here.
Indranil teaches public health, health economics, political economy and global health at OP Jindal Global University. He is an activist in Jan Swasthya Abhiyan.





