Diagnostics are an integral part of treatment and management of any disease. The track, test and treat strategy has become synonymous with COVID-19 pandemic control. Despite that, COVID-19 tests remain out of reach of the majority of the population in low and middle income countries (LMICs). The diagnostics pillar of the Access to COVID-19 Tools Accelerator (ACT-A) faces acute shortage of funds, does not have LMIC representatives and has set low targets for itself. The World Health Organization (WHO), on the other hand, has been conservative in promoting and approving rapid diagnostic tests (RDTs) which could boost testing in LMICs. The result — extended mass lockdowns and unchecked spread of COVID-19.
Tests: as important as vaccines
“Pandemic control measures like tracking, isolation and quarantine depend on testing. Diagnostics need to be easily available and free of cost for everyone to test whenever needed,” said Dr Ajay Verma, a medical doctor who has been on COVID-19 duty since last year in the All India Institute of Medical Sciences, Delhi, India. “However, containing the spread of infectious diseases depends a lot on proper use of tests,” he added, stressing the importance of rational use of diagnostics.
By diagnosing individual cases early and providing adequate care, countries can also find possible hotspots of virus spread. This would give more time to isolate them and diminish the space for transmission.
“The need for testing will remain even after vaccination due to the constantly emerging new variants. Even vaccinated people may get infected and they will need testing,” says Dr Fifa Rahman, the civil society representative in the ACT-A Diagnostics Pillar. She added that in absence of enough testing, governments will have to rely on mass lockdowns, while adequate testing would at least allow for more localized and brief lockdowns.
Nevertheless, the current diagnostics infrastructure seems to be far away from that ideal. Available data clearly shows extreme levels of inequality between countries. The Democratic Republic of Congo is able to have a testing rate of 22 daily tests per million, Uganda 80, and Mexico 225. Compared to that, Israel’s daily tests per million stands at 13206, United Kingdom’s is 10979 and for France, it is 8359.
ACT-A’s diagnostic pillar was established in April 2020 with exactly the idea of reducing this, much anticipated, inequality. The pillar is coordinated by FIND, a global alliance for diagnostics, and the Global Fund to fight AIDS, Tuberculosis, and Malaria. The original goal of the diagnostics pillar was to distribute 85 million tests in LMICs by the end of 2021. According to a progress report available on FIND’s website, however, for now merely 39 million tests were procured through ACT-A.
The donors’ bias
ACT-A’s vaccines pillar has attracted USD 12,278 millions in funds and it is reflected in the huge attention that production, regulation and distribution of vaccines has received. Diagnostics pillar, on the other hand, has received USD 1047 million, just 8% of the funds for the vaccines pillar. Discussions at ACT-A also show bias against funding for diagnostics. Presentation slides accessed by People’s Health Dispatch reveal that in a recent project to counter the Delta variant, the Rapid ACT Accelerator Delta Response (RADAR), diagnostics face the highest funding gap.
“Fundraising of ACT-A is very donor driven. Donors decide what they want to fund, and currently they’re not perceiving diagnostics or therapeutics being as interesting as vaccines,” says Rahman. The majority of the funding for diagnostics comes predominantly from governments, although some multilateral and private donors can be found on the list of funders.
Brook Baker, a professor at Northeastern University and civil society representative to ACT-A’s therapeutics pillar, agrees. He adds that by throwing their money behind the development of vaccines, rich countries and their private entities are prioritizing the protection of their own population and position of power. “Rich countries are approaching the pandemic with a colonialist bias: testing is not perceived as important as vaccination, because vaccines provide clearer-cut protection from importing the virus into their territories.”
Testing reluctance
Even so, there is no LMIC representation in the ACT-A diagnostics pillar. “The working group meets every two weeks,” says Rahman, “but it is only the Global North discussing the way forward.” The absence of LMICs in governance mechanisms such as the ACT-A diagnostics pillar has impacted their approach to local testing. Slow and sometimes unclear communications about the accuracy of test types has led to resistance towards a more widespread use of RDTs. RDTs require less time and laboratory capacities than polymerase chain reaction (PCR) tests that are still considered by many as the gold standard.
“Developing countries do not have the necessary laboratory infrastructure to base their testing campaigns on PCR tests. We should be focusing on RDTs as the technology is cheaper. As they do not require lab technicians, RDTs are adequate for low-resource settings. They are needed for understanding the spread of the virus in community settings. We need simple tests when they are required at such a large scale,” said Verma. A delay of even 3-4 days in getting test results can be harmful for a person and her surroundings.
WHO, however, promoted only PCR tests as the go-to option for a long time. Rich countries hoarded tests, leaving the rest of the world without. “Even after RDTs entered the scene, the WHO took a long time to incorporate them in its official guidance and promote their use. All of this has led to a sort of conservatism towards RDTs in LMICs,” says Rahman. A clear guidance by the WHO would have helped the developing countries in using more rapid tests, potentially making detention of COVID-19 easier.
“The WHO only recently added community testing in their guidelines, which is far too late,” said Rahman.
Baker says that despite repeated calls by civil society and scientists to adopt a “test and treat” approach to COVID-19, WHO has not done it so far. “They argue that there is no treatment so far and hence we can not go for test-and-treat the way we did for HIV and Hepatitis C,” informed Baker. However, he added, that test and treat is a broader concept. Infected people need to be tested fast and provided requisite care at the earliest to reduce mortality. WHO needs to be more radical in its approach, he said.
Diagnostics free in rich countries, out of reach in LMICs
Another serious problem that LMICs faced during the procurement of tests was pricing. At the beginning, individual PCR tests were priced at around USD 5, unaffordable for LMICs. More recent efforts by ACT-A has brought the price down to USD 2.50, which is still too high to ensure widespread testing.
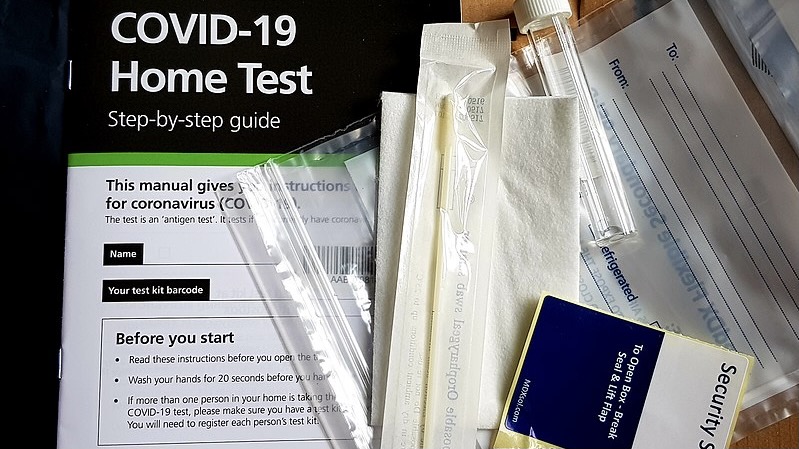
And while in LMICs testing is often provided though the private sector, meaning that the poorest are left without the space for regular testing, in many rich countries it is free of charge. In Germany, for instance, testing will be free for all until at least September 2021. Rich countries are also introducing easily accessible home kits for testing. Some people are testing as frequently as once a week if they feel the need. “As WHO continues to warn about the emergence and spread of new variants, it is crucial we make sure that these options are available in LMICs as well,” said Rahman.
To make sure more people are getting tested as new and more dangerous variants emerge, the world needs a radical shift from how it’s planning diagnostics at the moment. “It is about universal health care for every disease, including COVID-19. Everyone everywhere should have equal access to diagnostics free of charge to ensure rational treatment and management of the disease. The governments and international agencies can do much better than what they have done so far,” said Verma.